Date: May 21, 2025
Across the country, Skilled Nursing Facilities (SNFs) are seeing a noticeable rise in pressure injuries and wound-related complications. Patients are being discharged from hospitals sooner, often with complex conditions and active wounds. SNFs are now managing more acuity with fewer resources.
At the same time, the Centers for Medicare & Medicaid Services (CMS) continues to refine how it tracks and reports facility performance, including pressure ulcers, readmissions, and transitions of care.
Let’s explore why many SNFs are choosing to strengthen their wound care approach through collaborative partnerships.
The New Reality: Higher-Acuity Patients and Less Margin for Error
In today’s post-acute care environment, SNFs are expected to manage:
- Complex wounds on admission
- Co-morbid conditions like diabetes and vascular disease
- Patients with reduced mobility or post-surgical complications
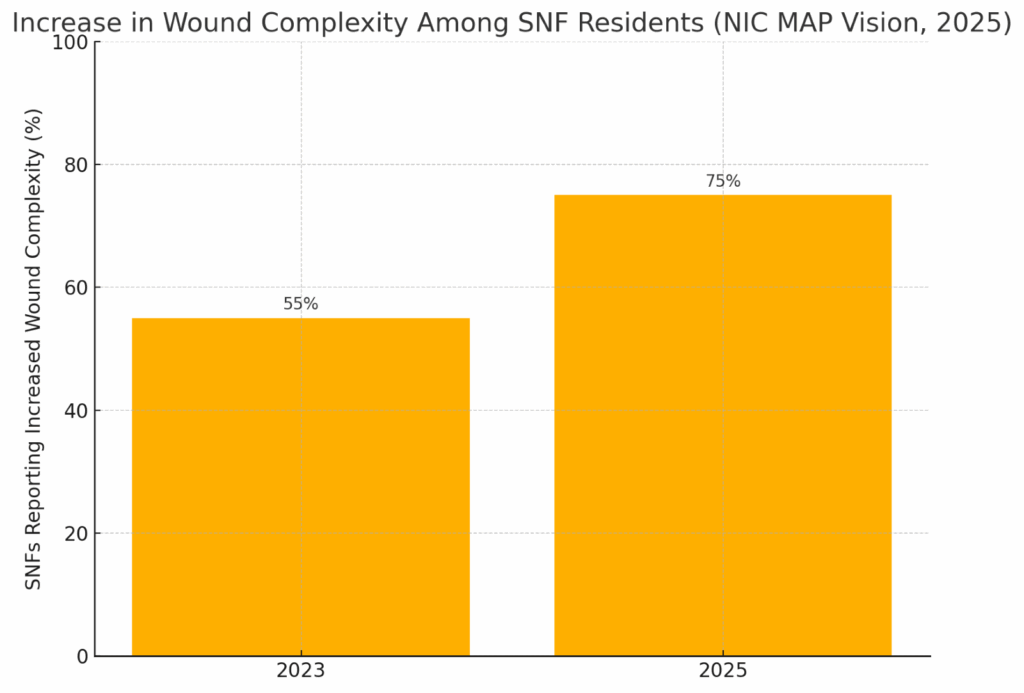
According to NIC MAP Vision, 75% of SNFs report increased wound complexity among incoming residents, a 20% rise compared to two years ago (source: NIC MAP Vision, 2025).
Even with strong internal nursing teams, the demands on staff are growing and so are expectations from regulators, families, and referral partners.
What CMS is Watching and Why It Matters
CMS (Centers for Medicare & Medicaid Services) tracks and publicly reports key quality indicators, including:
- Prevalence of pressure injuries in long-stay residents
- Hospital readmission rates
- Emergency department visits
- Discharge to community success
These indicators directly influence:
- Star Ratings
- Reimbursement
- Public trust
- Referral relationships
In recent updates to the SNF Quality Reporting Program, CMS emphasized closer monitoring of potentially avoidable hospitalizations, especially those linked to pressure injuries or wound-related infections (source: CMS.gov, 2024 SNF QRP Updates).
This is why many SNFs are proactively assessing how they manage wound care and realizing additional support improves both patient care and facility performance.
See how we work with our partners
The Challenge: Meeting Wound Demands with Limited Bandwidth
We truly understand that wound rounds are a vital part of every facility’s care model. But when patient acuity rises and staffing remains tight, even the most experienced teams may face constraints.
Common challenges we hear from our partners in Skilled Nursing/Long Term Care include:
- Staffing concerns when wound care needs to be addressed outside of the facility.
- Difficulty mobilizing patients to seek advanced care.
- Stress on the SNF team
- Increased costs associated with transporting patients.
- Limited access to advanced wound imaging or vascular assessment tools
- Difficulty obtaining timely specialist input for complex or non-healing wounds
At RFH, we know that none of these reflect a lack of dedication, they reflect a care environment that’s evolving faster than staffing or technological resources can keep up.
That’s where outside support, like working with an advanced wound care partner, can add meaningful value not by taking over, but by enhancing your existing team with tools and bandwidth that support better healing.
Why SNFs Are Partnering with Mobile Wound Care Teams
At Restore First Health, we work with SNFs as an extension of their clinical team, not a replacement.
Restore First Health’s model brings:
- Advanced bedside wound evaluation
- Auto-fluorescent imaging to visualize bioburden
- ABI studies to assess vascular status
- Advanced therapeutic dressings and healing
- Coordination with SNF wound nurses and DONs
- Documentation that aligns with your EMR and care protocols
We tailor our involvement based on each facility’s needs — ensuring your team stays in the loop, and your patients receive the highest standard of care.
The Results: Stronger Collaboration, Better Healing
Based on our 2024 internal outcomes data:
- 56% of diabetic foot and venous stasis ulcers healed within 12 weeks under Restore First Health’s mobile wound care program (source: Restore First Health Outcomes Report, 2024)
DOWNLOAD A RECENT CASE STUDY OF HOW A MAN WENT FROM FACING AMPUTATION TO FULLY HEALED IN JUST 9 WEEKS:
- Our partnered facilities have reported fewer wound-related readmissions, improved wound tracking, and higher family satisfaction scores.
The key? Consistent communication, shared decision-making, and seamless integration into your existing processes.
Moving Forward: A Proactive Step Toward Better Outcomes
As CMS continues to raise expectations and patient complexity continues to rise, partnering with an advanced wound care team can provide the support and tools your facility needs to stay ahead.
If you’re exploring ways to:
- Reduce wound-related hospitalizations and readmissions
- Improve healing timelines
- Support your nursing team with advanced tech and expertise
We’re here to collaborate.
Related video on The Truth on Diabetic Ulcers, from RFH:
References:
- CMS.gov. “SNF Quality Reporting Program Measure Calculations and Public Reporting.” Accessed April 2025. https://www.cms.gov/
- National Investment Center for Seniors Housing & Care (NIC MAP Vision). “Post-Acute Trends & Facility Complexity Report 2025.” Published March 2025.
- Restore First Health Outcomes Report, Internal Data 2024.
